If you are having IVF and have experienced frozen embryo transfer failure, you will be very frustrated.
Having undergone the process of ovarian stimulation and possibly a previous full IVF cycle using fresh embryos, only to find your pregnancy test negative after a frozen embryo transfer, you may feel despairing. The internet is awash with old wives’ tales about how to increase frozen embryo transfer success – from wearing warm socks to things to keep by your bed. But if you’ve experienced IVF failure or recurrent miscarriage, you will want more than old wives’ tales. Here we break down some of the potential reasons for failure and talk about possible ways to try to increase frozen embryo transfer success.
Why do my frozen embryo transfers keep failing and how can I increase frozen embryo transfer success?
If you are looking to increase frozen embryo transfer success, you will probably have encountered these basic tips:
- If you are older, or have experienced previous IVF failure, you might want to consider transferring more than one embryo (maybe)
- Make sure you have undergone thorough fertility screening (yes, it sounds obvious, but different test packages yield different levels of clarity)
- Consider taking folic acid and a good multivitamin
- Make sure your nutritional intake is good, with plenty of foods for fertility
But what about beyond that? Let’s take a look in more depth at some of the issues that can cause implantation failure:
Embryo problems
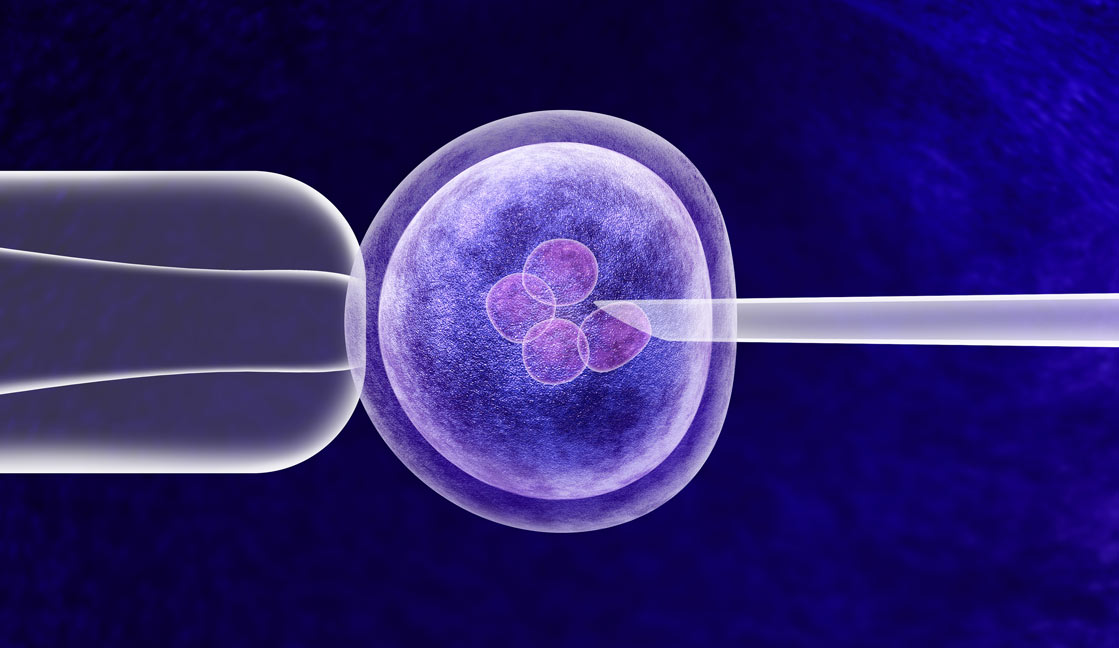
After fertilisation in the lab (‘in-vitro’ fertilisation), embryos are put into an incubator to grow and develop for between 2-5 days, with embryologists monitoring their progress so that only healthy-looking embryos can be selected for implantation/freezing.
Traditionally in IVF, embryos are retrieved from the incubator daily for observation, which may expose them to suboptimal conditions (like temperature variation). But some clinics make use of advanced time-lapse imaging technology to more closely monitor the embryos’ development without having to remove them from the incubator. Here at The Fertility and Gynaecology Academy we use a state-of-the-art embryoscope to monitor the embryos – an incubator with an in-built microscope and camera that captures images of the embryos every 10-20 minutes (time-lapse imaging). Carefully reviewing the pictures and video enables our fertility experts to select only the healthiest-looking embryos for freezing and implantation. You can find the HFEA view on time-lapse imaging here.
Genetic abnormalities in the embryo
The likelihood of genetic abnormalities in eggs and sperm grows as would-be parents get older. Genetic abnormalities in the embryo are frequently the cause of implantation failure and early miscarriage. And while IVF experts do everything they can to select the healthiest-looking embryos for implantation, even with highly sophisticated technology like the embryoscope we have here at The Fertility and Gynaecology Academy, unless we genetically test the embryos, we can’t be sure they don’t have problems like numerical chromosome abnormalities.
Some clinics, such The Fertility and Gynaecology Academy, can offer pre-implantation genetic testing on embryos in-house, to screen for abnormalities that cause implantation failure and miscarriage, allowing only normal embryos to be chosen for replacement into the womb. The HFEA view on genetic testing can be found here.
Failure to hatch
Fertilised eggs are encased in a hard outer layer (like a shell) named the zona pellucida. To be able to implant in the womb and become a pregnancy, the embryo must escape this shell. Sometimes an embryo fails to hatch and cannot implant in the womb. Assisted hatching is a process in which fertility experts make a tiny crack in the zona pellucida to try to help the embryo to break free and attach to the uterine wall, in order to develop into a pregnancy. The HFEA view on assisted hatching can be read here.
Uterine problems
Sometimes embryos fail to implant because there are undiscovered problems in the uterus, and so investigating and treating those problems may increase frozen embryo transfer success. Here at The Fertility and Gynaecology Academy, our wheelhouse is complex cases and we actually specialise in treating patients who’ve suffered recurrent miscarriage and recurrent IVF failure elsewhere. We often find problems such as:
Infection
Sophisticated screening is recommended for women experiencing recurrent implantation failure. Undiagnosed infections (for example chlamydia, mycoplasma, ureaplasma and more obscure issues) can create a hostile environment in the uterus, making it difficult for an embryo to implant or for your uterus to carry a baby to term. Infection (or endometritis) can also lead to hydrosalpinx, fluid in one or both fallopian tubes that can leak into the womb and disrupt the uterine lining, making it difficult for the embryo to implant.
Here at The Fertility and Gynaecology we can screen for common and obscure infections using not only vaginal swabs and semen but endometrial biopsy/menstrual blood, following up with scanning (and in the case of a problem like hydrosalpinx, surgery) if necessary.
Uterine cavity problems
Frozen embryo transfer can sometimes fail because of an abnormality in the uterine cavity, for example: scar tissue, polyps, adhesions or a septum. If this is suspected, doctors can investigate your uterine cavity by ultrasound (Aqua Scan/Saline Instillation Sonography), and then follow up with hysteroscopy to determine the best course of treatment. Treating uterine abnormalities can help to increase frozen embryo transfer success.
Hormonal imbalance
If the balance of hormones such as progesterone is suboptimal, it will make it more difficult for the embryo to implant in the uterine wall and develop into a pregnancy. To increase frozen embryo transfer success next time, your IVF doctor may for example need to assess and adjust the level of progesterone supplementation you are given.
Immune issues
“A woman’s immune system and reproductive system have a very complex relationship that science is still trying to understand,” says Dr Gorgy, Fertility Consultant at The Fertility and Gynaecology Academy. “Your incredible immune system defends you against foreign cells, ambushing invaders like viruses and even your cells if they become damaged. Pregnancy presents a conundrum: a woman’s immune system must at once not attack the embryo (which is made up of at least half foreign cells) whilst also guarding against viruses and infections that could disturb the embryo. For implantation and pregnancy to succeed, this foreign tissue must not be rejected. Some women have problems with immune cells and their reproductive system which may result in implantation failure or miscarriage.
Here at The Fertility and Gynaecology Academy we specialise in treating women who have suffered repeated IVF failure or recurrent miscarriage. Without giving false hope, we believe we can help such patients to increase frozen embryo transfer success by studying the role of their immune system in reproduction and offering any appropriate tailored immune treatments. This is known as reproductive immunology. You can read the HFEA view on reproductive immunology here.
Our specialism is treating complex cases. Couples frequently come to us after all but giving up hope, and we’ve helped countless such people finally achieve their dream of a baby of their own.
For help to increase frozen embryo transfer success or find out what the problem may be, call 020 7224 1880 or email info@fertility-academy.co.uk