If you’re considering assisted conception, you’re probably wondering what the IVF process involves.
At first glance it can seem like a minefield of acronyms and strange words and you may have questions like: Are IVF procedures painful? How long is the IVF process from start to finish? Read on and let’s demystify it all.
First things first – What is IVF?
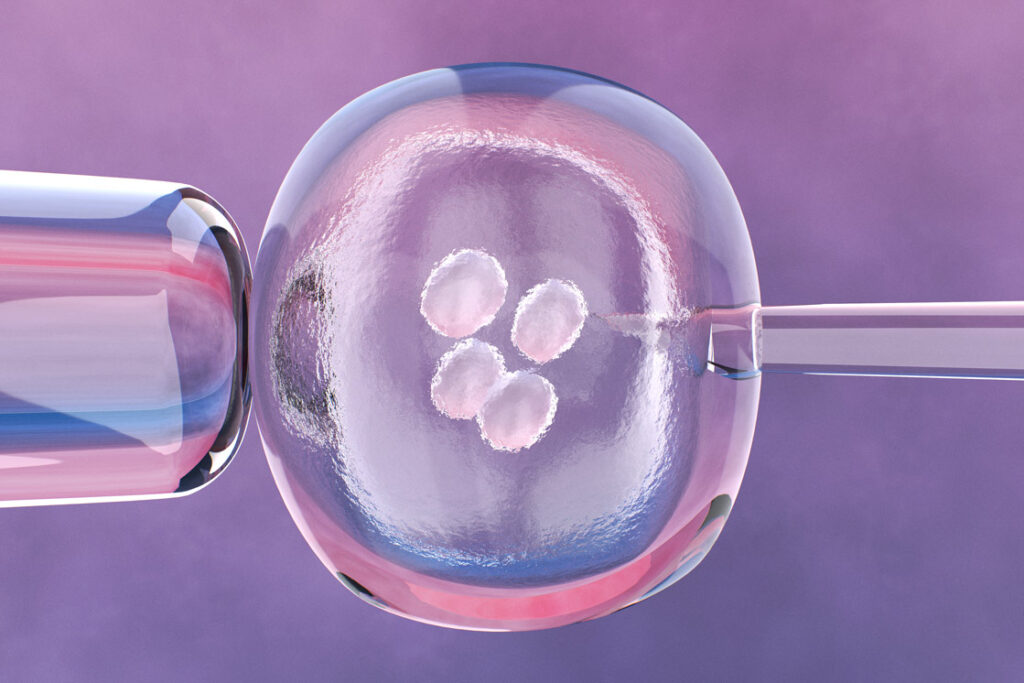
In-vitro fertilisation (IVF) is an assisted conception technique whereby a woman’s eggs are fertilised with sperm in a laboratory, before being placed back into the womb to grow and develop.
Dr Gorgy, one of the UK’s finest fertility doctors and co-director of The Fertility and Gynaecology Academy says: “There are different variations of the IVF process depending upon a couple’s needs and preferences. For example, if the male partner has sperm problems, then fertilisation should be conducted by injecting the sperm directly into the egg – this is called Intracytoplasmic Sperm Injection (ICSI). Or if the woman is older, assisted hatching may be suggested as an additional step in the IVF process. This is when the shell-like coating of an embryo is perforated in the lab, to help the embryo break out of this shell – which it must do in order to implant in the womb.”
A good fertility clinic will conduct exacting testing and consultation to get to the root of a couple’s fertility problems, identifying the best treatment variations before the IVF process begins.
Who can have IVF? Am I a candidate for IVF?
IVF may be suggested if you or your partner:
- Have blocked fallopian tubes
- Have age-related fertility decline such as low ovarian reserve
- Have an ovulatory disorder such as Polycystic Ovarian Syndrome (PCOS)
- Have tried unsuccessfully to conceive for three years
- Have a disorder such as endometriosis or pelvic adhesions
- Have sperm problems such as poor motility, abnormal sperm shape or low sperm count
- Have unexplained infertility for three years
- Have tried other less statistically effective assisted conception techniques (such as intrauterine insemination (IUI)) that have failed
- Are opting for surrogacy
If you are unsure, or you have been trying to conceive for a while without success, then it’s a good idea to visit a clinic for fertility testing. Time is fertility, so it’s important to get a handle on any potential roadblocks sooner rather than later.
The IVF process step by step
There are many potential variations in the IVF process depending on the individual needs and preferences of the couple at hand, so what follows is a general outline.
Step 1: Scanning and testing
You will have a scan and a blood test before hormone treatment starts, to ensure you have a good starting point for IVF.
Step 2: Suppressing ovulation
You’ll be given a drug that prevents your pituitary gland from governing your ovaries so that you don’t ovulate before it is time to collect your eggs. You’ll need to administer this drug daily yourself as an injection (you’ll be shown how to do so at the clinic).
Step 3: Stimulating your ovaries
A woman usually produces one egg per monthly cycle. But since it’s likely that not every egg will fertilise during the IVF process and not every embryo will implant, clinics want to stimulate the ovaries to produce more eggs to give you the best chance of success. This is called ‘controlled ovarian stimulation’. For this you will be given follicle stimulating hormone (FSH) to inject daily (you’ll be shown how to do this at home).
Step 4: Monitoring your progress and fine-tuning your response
Three to five days into your daily injections, you will undergo a blood test and a transvaginal scan to monitor the response of your ovaries to the hormones. After this, you will be scanned and have your blood taken every other day to modify the dose of your medication. It takes on average 10 to 12 days of injections until the eggs are suitably prepared.
Step 5: Final ‘trigger’ injection
Once your eggs are ready, you will be given a ‘trigger’ injection of a hormone called human chorionic gonadotropin (HCG) which matures the eggs ahead of their retrieval.
Step 6: Egg Collection
Egg collection will happen around 36 hours after the ‘trigger’ injection of HCG. You must not eat or drink anything from midnight prior to egg collection. You’ll be given intravenous sedation so you won’t feel anything. Transvaginally and with the aid of ultrasound guidance, your eggs will be collected via a needle going into the ovarian follicles. The procedure normally takes 15-20 minutes, and you can usually go home an hour or two after it’s completed. You must not drive for 24 hours, and you should have someone with you to take you home.
From the night following egg retrieval, you will need to start taking progesterone to prepare your uterus for implantation. The progesterone is taken either as intramuscular injection, gel, or suppositories.
Many women will experience bloating and some discomfort in their lower abdomen for a few days afterwards, as well as a bit of bleeding. It is better to use sanitary pads than tampons for the bleeding. Paracetamol can help, and you should drink plenty of water. It’s a good idea to rest and take the day following egg retrieval off work.
Step 7: Semen Production
The male partner will need to produce a semen sample – usually at the clinic. Prior to giving the sample, he will need to refrain from sex for 2-3 days but for no longer than 5 days.
Step 8: Egg Fertilisation
In the laboratory, your retrieved eggs will be mixed with the sperm for fertilisation after the semen sample is cleaned and filtered to concentrate the best sperm. In cases where there are sperm problems, the sperm may be injected directly into the eggs (intracytoplasmic sperm injection, or ICSI).
The embryos (fertilised eggs) will be left in the laboratory to grow, usually for between 2-5 days, and their progress will be monitored throughout. In fact here at The Fertility and Gynaecology Academy, we can use a state of the art embryoscope, which employs time-lapse imaging to capture the development of the embryos constantly, allowing us to pinpoint the very strongest embryos for implantation and offering the added benefit of not needing to take the embryos out of the incubator to check on their progress, which could expose them to suboptimal conditions.
Our embryologist(s) will assess the embryos and select the strongest 1 or 2 for transfer. If you are over 40 years old and using your own eggs, up to 3 embryos can be transferred.
The question of whether one or two embryos are transferred tends to depend on the age of the woman, how many (if any) IVF cycles she has already undergone, and how many high-quality embryos there are available.
Step 9: Embryo Transfer
A few days following egg retrieval, the embryo(s) will be placed into your uterus.
You should have a full bladder for the procedure, so drink a litre of fluid an hour beforehand. This is a more straightforward process than egg retrieval that can be likened to having a cervical smear test, so most women don’t need anaesthetic. The embryo(s) are placed into your uterus with the aid of a catheter passed through the vagina and cervix.
Step 10: Embryo freezing
If you have good quality embryos left over from the IVF process, they can be frozen and stored for any potential future fertility treatment. The law currently allows storage for up to 55 years, though both you and your partner must consent, pay for storage, and renew your consent every 10 years. For use in any future fertility treatment, the embryo(s) will be thawed when your uterine lining is ready.
Step 11: Resting and waiting
You should relax and take it easy in the period between the embryo transfer and the pregnancy test (about 14 days following egg collection), particularly in the period between embryo transfer and implantation (about 2 days following embryo transfer). You can undertake regular daily activities such as showering and walking around but you should refrain from strenuous activity and heavy lifting. Most couples prefer not to have sex until the pregnancy test although this is not necessary.
Step 12: Pregnancy test
About two weeks after egg collection, you will take a blood pregnancy test.
How long is the IVF process from start to finish?
Typically, an IVF treatment cycle is around 4-6 weeks until the pregnancy test.
How do I prepare for my first IVF?
Before you begin the IVF process, it’s a good idea to prepare your body by:
- Eating a healthy diet with plenty of vegetables and fertility foods
- Finding some decent prenatal vitamins
- Cutting out caffeine, smoking and alcohol
- Maintaining a healthy BMI
- Avoiding trips to destinations with a higher risk of infections that could delay your IVF treatment (for example zika virus)
- Having implication counselling
IVF can be very challenging emotionally too, so many patients find it helpful to support themselves mentally and emotionally before treatment in some of the following ways:
- Meditating
- Doing some yoga
- Having acupuncture treatment
- Journalling
- Trying a support group for people with fertility problems
Are IVF procedures painful?
Hormone injections: Pain-wise, you’ll generally only experience a short sting. But of course injections are more difficult for people with fear of needles. If you have a fear of needles, it may be helpful to mention that to your clinician at your consultation.
Egg retrieval: You will be sedated for egg retrieval so you will not feel any pain during the procedure. In the week following though, you may experience some cramping akin to menstrual pain, along with some soreness and spotting. You can take paracetamol for this.
Embryo transfer: This part of the IVF process is often likened to a smear test or ultrasound, so while women don’t relish it, it’s usually not painful. However, it’s common to experience some mild to moderate cramps in the few days following, which you can take paracetamol for.
What are the side effects and risks of IVF?
In the IVF process, it’s the hormone injections that tend to come with the most side effects, and common ones include:
- Mood swings
- Tiredness
- Headaches
- Hot flushes
- Bloating
- Nausea
- Reduced appetite or greater appetite
- Soreness or bruising around the injection site
- Lowered sex drive
- Breast soreness
Some women experience many of those side effects and others barely at all. Generally, women who’ve successfully conceived through IVF say the temporary side effects paled in significance to holding their very own baby in their arms.
In very rare cases, a woman may experience a reaction to the hormones known as Ovarian Hyperstimulation Syndrome (OHSS). This is when too many follicles grow, leading fluid to escape into the abdomen. Symptoms include nausea, diarrhoea, weight gain and bloating. OHSS can usually be resolved at home through hydration and lots of lying down. Very rarely in more severe OHSS, hospital treatment could be needed.
In an IVF process in which two or three embryos will be placed into the womb, there is a greater chance of multiple pregnancy, and multiple pregnancies carry greater risk of complications such as gestational diabetes and preeclampsia. In the earlier days of IVF, transferring more than one embryo in the IVF process was much more common. These days however, most IVF cycles will involve the transfer of just one embryo, because technological advancements have allowed us to be more precise in selecting the best quality embryos for transfer. In fact, we use an embryoscope with time-lapse imaging to monitor the development of the embryos with unbeaten care and closeness, selecting only the best for transfer.
Have you been trying to conceive for a while? Want to check if everything is alright? At The Fertility and Gynaecology, we’ve successfully helped countless couples who’d all but given up hope, to finally achieve their dream of a baby of their own. With state of the art technology and expertise second to none, we can guide you carefully through the IVF process every step of the way.
To find out more or book a consultation, call The Fertility and Gynaecology Academy now on 020 7224 1880 or email info@fertility-academy.co.uk.